Last Updated on December 3, 2024 by Helena Akter
With the ever-increasing healthcare costs, you might often find yourself asking, “Does insurance cover ambulance?” This question has become a pressing concern for many of us and our families. After all, medical emergencies can strike at any moment, and ambulance rides can pile up quickly, causing financial stress.
Insurance covers ambulance rides for emergencies and certain non-emergency scenarios if medically necessary. And coverage varies by policy and provider, including some car insurance plans. So, always check your policy for specifics on ambulance ride coverage.
In this piece, we’ll give you the information you need to understand ambulance coverage. You’ll learn the different costs of ground and air ambulance services, and we’ll show you which plan provides the ride coverage. So, finish it up!
Does Insurance Cover Ambulance Rides?
Your insurance usually has your back when it comes to ambulance rides in emergencies, and sometimes even in non-emergencies, if they’re medically necessary. But remember, the coverage can vary based on your specific policy and provider. It might even extend to some car insurance plans.
Just a heads up, even in urgent situations, like after a serious car accident where an ambulance is absolutely necessary, copays and deductibles may still apply.
Now, when we talk about ‘medical necessity’, it means you need immediate medical care while you’re on your way to the hospital. It could be situations where you’re having difficulty like —
- Breathing
- Experiencing chest pain
- Dealing with other severe conditions
that need a paramedic’s attention during your journey to the hospital. These scenarios are likely to be covered by your insurance.
You might also find it interesting to know that in 2022, the No Surprises Act was introduced to help reduce unexpected medical bills. It covers emergency and certain non-emergency services, including aftercare for emergencies.
But, it’s important to note that this act doesn’t apply to ground ambulance services.
What is the Cost of an Ambulance Ride?
Recently, healthcare costs got so high and an ambulance ride can be surprisingly expensive. And it’s not just because of the vehicle’s cost, which can exceed $250,000. The price also covers life support, medication, and medical care you might need during the ride.
Typically, the cost ranges from a few hundred to several thousand dollars. The final amount you pay depends on various factors:
- Location: Costs can vary widely depending on where you are in the country.
- Distance of the trip: Charges often include a fee per mile, so longer distances mean higher costs.
- Medical care during the trip: Any treatment or medication you receive in the ambulance adds to the bill.
- Type of transport: Air ambulance services cost much more, sometimes reaching tens of thousands of dollars.
For instance, in Irving, Texas, someone under 65 would pay $750 for basic life support, plus 30% more for any used consumables, $15 for each mile travelled, and a $5 technology fee. Meanwhile, in California, the average ambulance ride costs $589.
What Types Of Transport are Covered by Health Insurance Plans?
Health insurance usually pays for emergency rides to the closest hospital that can handle your condition. They might also cover rides that aren’t emergencies, such as —
- Moving you from a hospital that’s out of your insurance network to one that’s within the network, if you need medical services.
- Transferring you from a short-term care facility to a long-term one for ongoing care.
- Taking you to another hospital in your network if the first one can’t give you the necessary treatment.
- Moving you from a hospital to a rehab center when you need more medical care.
These transports ensure you get the right care at the right place, covered by your insurance plan.
Does Car Insurance Cover Ambulance Rides?
If you ever find yourself in a crash, your car insurance could potentially cover the cost of your ambulance ride. It’s usually the case if you have coverage for medical payments (also known as MedPay) or personal injury protection (PIP).
You should know that PIP is often a requirement in states that follow no-fault insurance laws. Now, after a vehicle accident, both MedPay and PIP cover your medical expenses, which includes ambulance rides —
- PIP helps pay for medical bills from a car accident, like ambulance rides, medical expenses, lost income, rehab costs, and your health insurance deductible.
- MedPay covers ambulance fees, your health insurance deductible and copays, hospital visits, rehab, surgeries, X-rays, and more.
If you have MedPay or PIP and also health insurance, you usually need to use your car insurance first for ambulance ride costs after an accident. Your health insurance might cover ambulance rides, but your car insurance is the first one to turn to.
After that, you can ask your health insurance to pay for any medical costs not covered by your car insurance. For ambulance rides and other accident-related costs, you can ask the other driver’s liability insurance for payment if you don’t have MedPay or PIP.
What Types of Car Insurance Cover Ambulance Rides?

After a car crash, different types of car insurance might help cover the cost of an ambulance ride. However, not every insurance type covers this in every situation, and availability varies by state.
Here are the types of car insurance that might cover ambulance rides —
- Personal Injury Protection (PIP): In states with no-fault laws, PIP covers your medical bills, including ambulance fees, no matter who caused the crash.
- Medical Payments (MedPay): This optional coverage pays for ambulance rides similarly to PIP and is available where PIP isn’t required or as an addition to it.
- The Other Driver’s Bodily Injury Liability: If the other driver is at fault, their insurance should pay for ambulance services and other medical expenses.
- Underinsured or Uninsured Motorist Coverage: If the at-fault driver lacks insurance or doesn’t have enough to cover your bills, this coverage steps in. It’s optional in some places and mandatory in others.
Does Cigna Cover Ambulance Rides?
Cigna health insurance does cover —
- Ambulance rides are needed for emergencies.
- Ambulance services for those waiting for a transplant.
- Rides for patients needing special medical care during the trip or those who must stay in bed and need to go to another medical center.
- For urgent or time-sensitive transplants, Cigna will also cover ambulance transportation if there are no other transportation options available.
Does Anthem Cover Ambulance Rides?
Anthem, offering certain Blue Cross Blue Shield (BCBS) health plans, provides ambulance rides to nearby medical facilities. It includes the ambulance’s base charge, parking, mileage, and wait times.
However, Anthem does not cover —
- Miles traveled by ambulance without a patient.
- Charges for treatment when the patient isn’t transported.
- Travel costs for a caregiver.
- Extra miles to a facility farther than the nearest suitable one.
Does UnitedHealthcare Cover Ambulance Rides?
UnitedHealthcare health insurance plans do cover —
- Emergency ambulance services by licensed providers to the nearest hospital for needed treatment.
- Most non-emergency transfers between medical facilities.
- For emergency rides with out-of-network ambulance services, UnitedHealthcare will cover your deductible or copay as for in-network services.
Does Kaiser Permanente Cover Ambulance Rides?
Kaiser Permanente health insurance provides coverage for —
- Ambulance transport in life-threatening emergencies where delay could lead to serious health issues.
- Non-emergency ambulance rides if a doctor approves or if your health condition necessitates ambulance transportation.
- Kaiser Permanente excludes coverage for transport by car, taxi, gurney van, wheelchair van, or services not provided by licensed ambulance companies.
When Does Insurance Not Cover Ambulance Rides?
Health insurance doesn’t always pay for ambulance rides, especially in non-emergency cases. Some plans might cover non-emergency rides if they’re medically necessary and use in-network providers. That’s why you need to know the dos and don’ts when completing an individual health insurance application.
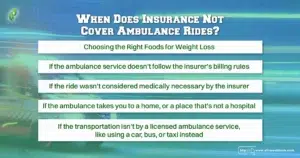
Here are reasons your insurance might not cover an ambulance ride —
- If you didn’t get approval from your insurance beforehand.
- If the ambulance service doesn’t follow the insurer’s billing rules.
- If the ride wasn’t considered medically necessary by the insurer.
- If the ambulance takes you to a home or a place that’s not a hospital.
- If the transportation isn’t by a licensed ambulance service, like using a car, bus, or taxi instead.
If it’s not an emergency, you should check with your insurance provider before arranging a ride.
What If Health Insurance Denies Coverage for an Ambulance Ride?
If your health insurance doesn’t cover an ambulance ride to the hospital, you can challenge the decision. Here’s how to go about it —
- First, reach out to your insurance provider to understand why they denied your claim. It might be because the type of ambulance service wasn’t covered, or the service didn’t document your medical needs correctly.
- Next, talk to the ambulance service. They might need to submit more information to support your claim.
- Then, if your claim is still rejected, start an appeal. Your insurance has specific rules and deadlines for appeals. You can find a sample appeal letter from the National Association of Insurance Commissioners.
- Follow up with your insurance if you don’t hear back within their response timeframe.
- If denied again, you might be able to ask for an external review. Your insurance company can tell you how to request this.
- Still, denied? Contact your state’s Department of Insurance, Attorney General, or Consumer Affairs office. They can assist with an external review.
If you’re facing high charges, like out-of-network rates, and your appeal succeeds, these state offices can also help. Many states have laws to protect you from unexpected ambulance bills.
Conclusion
So, does insurance cover ambulances? When an ambulance is needed in an emergency or in some non-emergency situations, your insurance usually covers the costs. However, you must know what your insurance covers when it comes to ambulance rides, especially in emergency situations.
Well, we tried to help you understand the ins and outs of your insurance policy’s ambulance coverage. Ultimately, it’s all about making sure you know what’s included in your plan before you actually need it. Knowing your policy’s finer details can prevent surprise bills and prepare you for any situation.
If you need more details, review your insurance documents or contact your provider. They’re there to help you understand more.
FAQs
How Much Does an Ambulance Cost in the USA Without Insurance?
Without insurance, an ambulance ride typically costs around $1,200. The No Surprises Act, designed to prevent unexpected medical bills, doesn’t apply to ambulance services. This means you’ll have to pay the full bill yourself.
What is a Deductible?
A deductible is what you must spend out of pocket for health care prior to your insurance starts covering some of the costs.
Does Medicaid Cover Ambulance Rides?
Yes, Medicaid covers emergency ambulance services provided by licensed companies. It also pays for non-emergency transports if a doctor orders it.
What is Coinsurance?
Once you’ve reached your deductible, the part of the costs for a covered healthcare service that you’re responsible for is known as coinsurance. It’s normally a percentage. For example, you might pay 20% of the price of a service, while your insurance covers the remaining 80%.
Does Medicare Cover Ambulance Rides?
Medicare Part B covers ambulance rides in emergencies, whether on the ground or in the air. It also covers some non-emergency ambulance services, but only if a doctor writes an order for it.

